Medical billing isn’t for the faint of heart. The challenges in medical billing—claim denials, rejected payments, endless paperwork, and ever-changing regulations—can turn the process into a constant headache. And if it’s not handled correctly? Delayed payments, compliance fines, and mounting frustration are just the beginning.
The good news? Most billing issues have simple fixes. You just need to know what to look out for and how to get ahead of them. Let’s dive into five of the most common challenges in medical billing—and what you can do to keep things running smoothly.
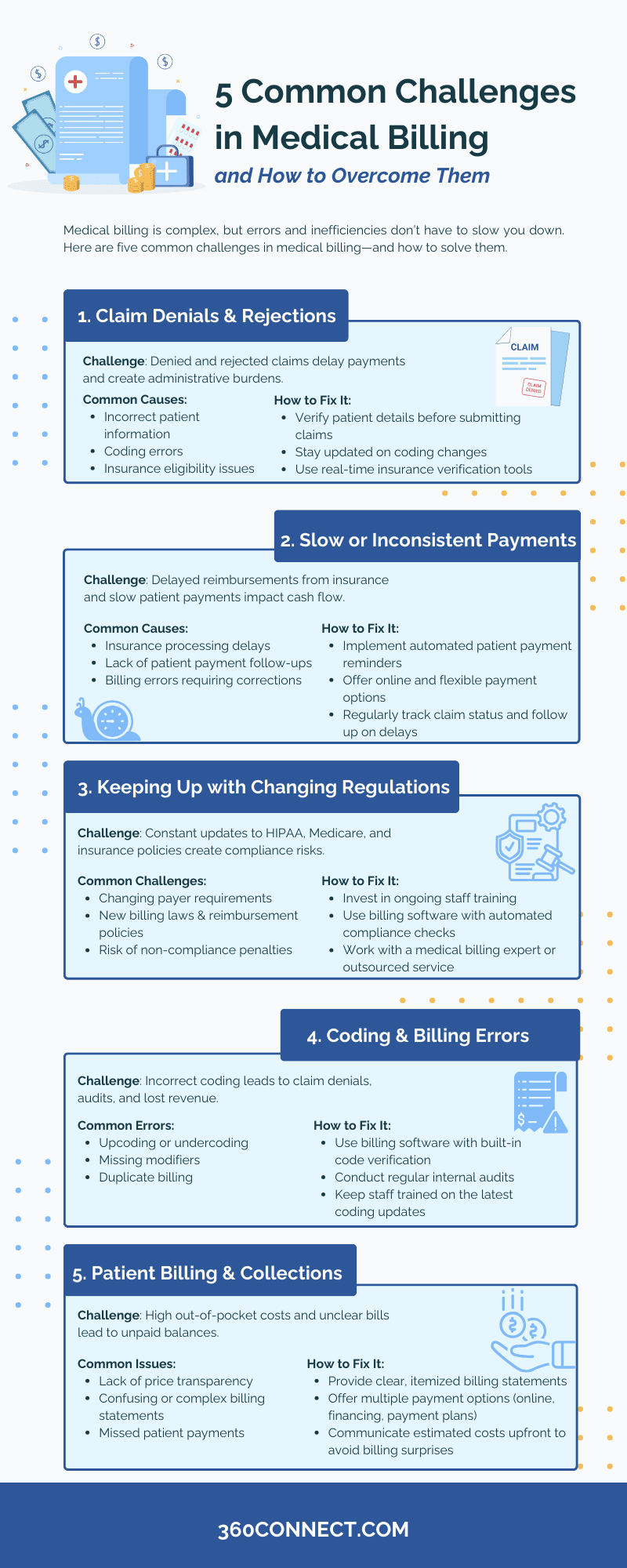
1. Claim Denials and Rejections: A Major Challenge in Medical Billing
Few things are more frustrating than submitting a claim only to have it denied or rejected. Unfortunately, it happens all too often. A denied claim means the insurance company has processed it but refuses to pay due to an issue, while a rejected claim is returned before processing because of errors. Either way, both can cause cash flow disruptions and require additional time to fix and resubmit.
The truth is, many claim denials stem from preventable errors. Whether it’s incorrect patient information, coding mistakes, or a lapse in insurance coverage, these issues add unnecessary delays to reimbursements and create administrative headaches for medical staff. That’s why overcoming challenges in medical billing starts with understanding common claim errors.
Common Reasons for Claim Denials:
- Incorrect or incomplete patient information – A simple typo in a name, birth date, or insurance ID can lead to rejection.
- Coding errors – Using outdated or incorrect CPT, ICD-10, or HCPCS codes can cause automatic denials. (32% of respondents named coding as their top concern in a study.)
- Insurance eligibility issues – If coverage has lapsed or the procedure isn’t covered under the patient’s plan, the claim may be denied.
How to Overcome It
Ensuring claims are submitted accurately the first time can reduce the risk of denials and speed up reimbursement.
- Verify patient information upfront – Always double-check patient demographics and insurance details before submitting claims.
- Stay updated on coding changes – Regular training for medical coders and billers can help prevent coding errors.
- Use real-time eligibility verification tools – Confirm insurance coverage before services are rendered to avoid claim issues later.
2. Slow or Inconsistent Payments
Medical practices depend on steady cash flow, but billing delays and inconsistent reimbursements can create financial strain. Between slow-paying insurance providers and patients struggling with medical bills, keeping revenue flowing smoothly is a challenge.
A significant reason for slow payments is a lack of transparency in the billing process. Patients may not fully understand their financial responsibility, while insurance carriers often have lengthy processing times.
Related: How to Streamline the Payment Process for Patients
Common Causes of Slow Payments:
- Delayed insurance processing – Some insurers take weeks to process claims, leading to gaps in cash flow.
- Lack of patient payment follow-ups – Patients may forget about unpaid balances if there’s no reminder system in place.
- Billing errors causing rework – Even minor errors in claims can lead to back-and-forth corrections and resubmissions, delaying payment further.
How to Overcome It
Reducing payment delays requires clear communication, follow-ups, and proactive billing strategies.
- Implement automated reminders – Send electronic reminders via email or text to prompt patients about outstanding balances.
- Offer flexible payment options – Allow patients to pay online, set up payment plans, or use financing solutions.
- Monitor claim status regularly – Use billing software to track claims in real-time and follow up with insurers on delayed payments.
3. Keeping Up with Changing Regulations
Medical billing isn’t just about submitting claims—it’s about staying compliant with ever-evolving regulations. One of the biggest challenges in medical billing is keeping up with frequent updates to HIPAA requirements, Medicare policies, and payer guidelines.
For example, surprise billing laws and value-based care models have changed how providers bill for services. Without regular updates, billing teams may struggle to submit claims correctly, leading to legal risks and revenue losses.
Common Regulatory Challenges in Medical Billing:
- HIPAA and data security requirements – Ensuring patient information remains secure and compliant with privacy laws.
- Medicare and Medicaid billing changes – New rules can affect reimbursement rates and eligibility.
- Evolving payer policies – Insurance companies frequently update coverage requirements, making it difficult to keep up.
How to Overcome It
Proactive compliance strategies can help prevent costly errors and legal complications.
- Invest in continuous education – Regular training for staff ensures they stay informed about regulation changes.
- Use compliance-focused billing software – Many systems now include automated compliance checks to reduce errors.
- Partner with a medical billing expert – Outsourcing to professionals who specialize in compliance can alleviate regulatory burdens.
4. Coding and Billing Errors
Even experienced medical coders make mistakes, but in billing, those errors come with a price. Challenges in medical billing often stem from coding mistakes that result in claim denials, delayed payments, and even audits if discrepancies become a pattern. When errors go unnoticed, they can cost a practice thousands in lost revenue or even compliance penalties.
A staggering 80 percent of hospital bills contain errors, highlighting how common billing inaccuracies are in the healthcare industry. These mistakes can stem from manual data entry, outdated coding knowledge, or simply the complexity of medical billing regulations.
Common Coding Mistakes:
- Upcoding or undercoding – Entering incorrect codes that either exaggerate or understate services provided.
- Missing modifiers – Not adding necessary billing modifiers can lead to rejected claims.
- Duplicate billing – Accidentally submitting the same claim twice, which can trigger an audit.
How to Overcome It:
A structured approach to coding can significantly reduce errors and prevent revenue loss.
- Utilize medical billing software with built-in code verification – This helps flag potential errors before submission.
- Conduct regular coding audits – Periodic reviews can identify patterns of mistakes and areas for improvement.
- Ensure ongoing coder education – Keeping staff trained on the latest coding updates reduces preventable errors.
5. Patient Billing and Collections
With high deductibles and increasing out-of-pocket costs, patient billing has become a growing challenge for healthcare providers. Many patients struggle to pay medical bills in full, while others may not prioritize medical debt, leading to outstanding balances.
Additionally, unclear billing statements often lead to confusion, making it harder for patients to understand what they owe and why.
Common Issues with Patient Billing:
- Lack of price transparency – Patients don’t always know what to expect when they receive their bill.
- Delayed or missed payments – Without clear communication, patients may not pay on time or at all.
- Complicated billing statements – Hard-to-read bills cause frustration and payment hesitations.
How to Overcome It:
Making the patient payment experience seamless and transparent can improve collection rates.
- Provide clear, itemized bills – Patients should easily understand charges and insurance contributions.
- Offer multiple payment options – Digital payments, payment plans, and financial assistance programs make it easier for patients to pay.
- Improve front-end communication – Informing patients of expected costs upfront reduces billing surprises and payment delays.
Final Thoughts on Common Challenges in Medical Billing
Medical billing challenges may seem overwhelming, but with the right strategies in place, they’re entirely manageable. By focusing on accuracy, compliance, and clear communication, healthcare providers can avoid common billing pitfalls and maintain a steady revenue stream.
If your practice is struggling with claim denials, slow payments, or outdated billing processes, it might be time to explore better solutions. Investing in advanced billing technology or outsourcing to a reliable billing partner can make all the difference.
Further Reading:
Get Medical Billing Quotes Now!
Navigating the complexities of medical billing doesn’t have to be a constant battle. Whether you’re dealing with frequent claim denials, slow reimbursements, compliance concerns, or patient payment challenges, the right billing solution can make all the difference. That’s where 360Connect comes in.
At 360Connect, we help healthcare providers find top-rated medical billing solutions tailored to their needs. Whether you’re looking to streamline your in-house billing process or outsource to a trusted billing service, we connect you with providers that can help.
How It Works:
- Tell us your needs – Answer a few quick questions about your practice.
- Get matched – Receive up to five free quotes from vetted medical billing providers.
Don’t let billing challenges hold your practice back. Take control of your revenue cycle today.

